- Home
- Medications
- Drugs for Treatment of Migraine
Drugs for Treatment of Migraine: Best Acute Migraine Medications
When a migraine attack strikes, you need relief as quickly as possible. The drugs for treatment of migraine that doctors recommend depend on the severity of your attack, how quickly your symptoms build, and whether you can tolerate oral medication.
This article explains the main options for acute migraine treatment - from over-the-counter pain relievers to triptans, ergotamine's, and fast-acting rescue medications sometimes used in the emergency room. It’s designed to help you have an informed, productive conversation with your doctor about the best plan for you.

Tip: Many people find it helpful to keep a medication plan written down. If you’d like one ready-made, you can grab my Printable Migraine Medication List - a quick tool to track what you’ve tried and discuss with your healthcare team.
Disclaimer: This information is for educational use only, not medical advice. Always consult your doctor for treatment protocols and before using any medication.
Scroll down for a detailed list you can download. First let's look at treatment by situation.
Early / Mild Drugs for Treatment of Migraine
For people with milder migraine attacks or when symptoms are caught early, over the counter (OTC) medications are often the first step. These can reduce pain and sometimes stop the attack from progressing if taken quickly enough.
Common first-line options include:
- Aspirin (600–900 mg initially, then 600 mg every 4 hours as needed)
- Paracetamol (Acetaminophen) 1000 mg, repeated every 4 hours (maximum 4 g per day)
- NSAIDs such as Ibuprofen (400–1200 mg), Naproxen (750–1250 mg), or Diclofenac (50–100 mg)
Tip: Taking medication at the very first sign of migraine - ideally within 30 minutes of symptom onset, usually improves effectiveness.
Combination treatments may help: some people find better relief when OTC pain relievers are paired with caffeine or an anti-nausea medication such as:
- Metoclopramide (10 mg) - helps with nausea and speeds stomach emptying so migraine drugs absorb faster
- Prochlorperazine (5 mg) - stronger for nausea, but may cause sedation (which can be desirable for some patients)
Important cautions:
- Avoid NSAIDs if you have kidney disease, stomach ulcers, or certain cardiovascular risks.
- Do not exceed the daily maximum dose of acetaminophen (4 g/day) to avoid liver damage.
- Frequent use of OTC medications (more than 10–15 days per month) can lead to medication-overuse headache (MOH).
If OTC medications aren’t effective, or if your attacks escalate quickly, your doctor may recommend moving to prescription acute treatments such as triptans or ergotamine's (see next section).
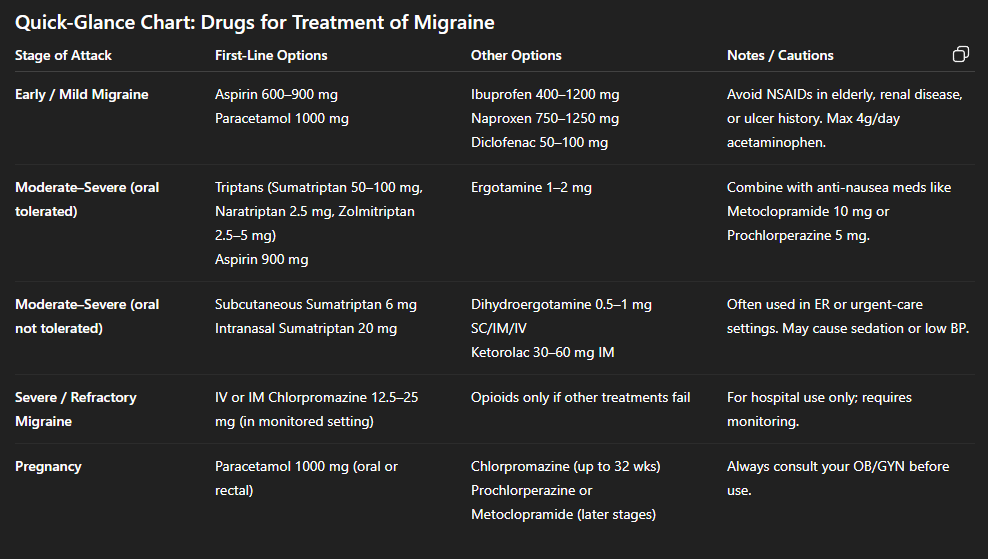
Before I go onto the next situation, here are some more details (you know I love to provide details) to help you understand the drugs for treatment of migraine from the Australian based NSW Therapeutic Advisory Group (TAG).
They have provided a fantastic summary on exactly what medications to take during an acute attack.
While this list is old, it is a fantastic resource to provide the medication options for migraine at each stage of severity. Your doctor may want to test the older, reliable medications before the newer CGRPs, gepants and ditans.
The levels of evidence were mostly obtained from review of randomized controlled trials or from experts in this field. Please click on this link to download the PDF to see even more details.
Now this table is hard to read on mobile, but I want you to have this information right now.
Stage of Migraine |
Recommendation |
Other Options |
|
Early / mild migraine |
Aspirin 600-900mg initially followed by 600 mg every 4 hours Paracetamol 1000mg every 4 hours (max 4g Paracetamol per day) Prochlorperazine 5 mg orally |
Naproxen 750 - 1250mg |
|
Persistent / moderate to severe migraine Able to tolerate oral medication |
Aspirin 900 mg followed by Aspirin 600 mg every 4 hours OR to 100 mg a second dose will NOT be effective)*
Metoclopramide 10 mg orally or prochlorperazine 5 mg orally |
Naratriptan 2.5mg orally |
|
Persistent / moderate to severe migraine Unable to take oral medication |
Dihydroergotamine 0.5-1mg SC, IM or IV 12.5mg IM
*see general discussion |
Ketorolac 30-60mg IM* |
|
Severe migraine and patient has taken ergotamine or triptan without effect |
If in a monitored environment Chlorpromazine 12.5-25mg IV or IM* (Note sedative and hypotensive effects. IM injection can cause sterile abscesses).
|
Ensure adequate hydration |
|
Migraine during pregnancy |
Paracetamol 1000mg orally or rectally every 4 hours |
Ensure adequate hydration |
This TAG article does not recommend Pethidine or Lignocaine for migraine attacks. As I mentioned, the paper is quite old now, 2002, but these drugs for treatment of migraine are all still widely used. I think it's important you know about everything that's available to you.
>> Download: Printable List of Migraine Medications - $4.99 to take to your doctor.
Now, let's get to the other treatments by situation...
Moderate to Severe Migraine (When Oral Meds Are Tolerated)
When a migraine attack is more intense and OTC options are not enough, doctors often recommend prescription medications designed to specifically target migraine pain. These work best when taken as soon as symptoms begin.
1. Triptans (first-line prescription treatment)
Triptans are migraine-specific drugs that work by targeting serotonin receptors in the brain to reduce inflammation and constrict blood vessels. They are the most commonly prescribed acute migraine drugs for moderate to severe attacks.
Common options include:
- Sumatriptan (Imitrex) 50–100 mg orally
- Naratriptan (Amerge) 2.5 mg orally
- Zolmitriptan (Zomig) 2.5–5 mg orally
Note: If sumatriptan 50-100 mg does not work the first time, a repeat dose usually won’t help. Other triptans may be tried instead.
Triptans are generally well tolerated but should not be used by people with certain heart or vascular conditions.
2. Ergotamine's (second line, less commonly used today)
- Ergotamine 1–2 mg orally (not exceeding 10 mg per week)
Ergot derivatives can be effective but carry a higher risk of side effects compared to triptans. They are sometimes used if triptans fail but are now prescribed less often due to newer options like gepants.
3. Combination with Anti-Nausea Medication
Even when oral medications are possible, nausea and vomiting can make drug absorption unreliable. Doctors often recommend pairing acute migraine drugs with an antiemetic:
- Metoclopramide 10 mg orally
- Prochlorperazine 5 mg orally
These not only reduce nausea but can help migraine drugs work faster.
Key things to discuss with your doctor:
- Which triptan is best for your specific migraine pattern and health history
- How many days per month it’s safe to use acute migraine medications
- When to move from oral to injectable or nasal options if attacks escalate quickly
Moderate to Severe Migraine (When Oral Medications Aren’t Tolerated)
For many of us, nausea and vomiting make swallowing tablets impossible during a severe migraine attack. In these cases, non-oral acute migraine drugs are used because they bypass the stomach and act faster.
1. Injectable Medications
Sumatriptan 6 mg subcutaneous (SC) injection
- Relief can occur within 10–15 minutes
- A second dose may be given after 1 hour only if the first dose was effective
Dihydroergotamine (DHE) 0.5–1 mg SC, IM, or IV
- Often paired with an anti-nausea drug such as metoclopramide
Remember... ask your doctor, as new medications are being approved often.
2. Nasal Sprays
Fast-absorbing through the nasal passages:
- Sumatriptan 20 mg intranasal spray
- Zolmitriptan 5 mg intranasal spray
- DHE intranasal (Migranal®)
These options are especially useful if you experience rapidly escalating attacks or severe nausea.
3. Suppositories
Prochlorperazine suppositories are useful when vomiting prevents oral absorption.
4. IV or IM Medications in a Monitored Setting
For very severe or prolonged attacks:
- Chlorpromazine 12.5–25 mg IV or IM (powerful, but requires monitoring due to sedation and low blood pressure risk)
- Ketorolac 30–60 mg IM (NSAID option when oral drugs aren’t possible)
These are usually administered in a clinic or hospital setting.
When to Consider Non-Oral Rescue Drugs:
- Repeated vomiting during attacks
- Very fast onset migraines where oral meds don’t act quickly enough
- Previous poor response to oral triptans or NSAIDs
Ready to take control of your migraine treatment?
Severe or Refractory Migraine (When First-Line Drugs Fail)
Sometimes a migraine does not respond to first-line treatments like NSAIDs, triptans, or DHE. These are called refractory migraines. At this stage, stronger medications - usually given in a clinic or emergency room - may be considered.
1. Chlorpromazine (Thorazine®)
- Given IV or IM under monitoring
- Can be as effective as DHE, ketorolac, or even triptans in small studies
- Risks: sedation, low blood pressure, sterile abscesses (if given IM)
2. Ketorolac (Toradol®) Injection
- 30–60 mg IM
- A powerful NSAID used when oral NSAIDs aren’t possible
- Avoid in patients with kidney issues or stomach ulcers
3. Other Options Sometimes Used in Hospitals
- IV fluids for dehydration (which can worsen migraine)
- IV steroids (dexamethasone) to help prevent recurrence after discharge
- Opioids are not recommended except as a last resort when all else fails, due to high risk of medication overuse headache and dependence.
4. Migraine in Pregnancy
- First-line: acetaminophen or paracetamol (safe in all trimesters)
- Chlorpromazine or metoclopramide may be considered under medical supervision
- NSAIDs and triptans are usually avoided, especially in the third trimester
Key Point: These treatments are generally reserved for hospital settings. If your migraine symptoms suddenly change or become extreme (e.g., thunderclap headache, neurological changes, fever), you should seek emergency care immediately.
How to Get Better Results from Your Acute Migraine Medications
Even the most effective drugs for the treatment of migraine won’t work well if they aren’t used correctly. Here are evidence-based strategies to help you get the best results:
1. Treat Early
Discuss early treatment to reduce as many symptoms as possible and cover self-management of your acute medications with your doctor.
- Take your acute medication as soon as you recognize migraine symptoms (aura or early pain).
- Early treatment is more likely to stop the attack or reduce its severity.
2. Work With Your Doctor on a Clear Plan
Prepare a treatment strategy with your doctor. If they do not have a plan, you will find a great one to use here in my post migraine pain medication.
- Ask your doctor to create a step-by-step acute treatment strategy (e.g., NSAID → triptan → rescue injection if needed).
- Review this plan regularly to see if changes are needed. If your episodes are frequent to discuss if you need prophylactics.
3. Track Your Results
Ask your doctor specifically how to measure your results and what to watch for from what they prescribe for you.
In order to determine the efficacy of the drugs for treatment of migraine you are trialing...
Keep a record of:
- How quickly the medication worked (note time to pain phase)
- Whether the pain was fully relieved or only reduced
- Any breakthrough pain or side effects
Use a simple 1-10 pain scale or a tracker app or check out my symptom tracker.
4. Watch for Medication Overuse Headache (MOH)
Keep a list of your symptoms and any “overlapping pain syndromes” after the migraine attack. Things like a tension headache, or possible rebound headache from your prescribed drugs for treatment of migraine or over the counter painkillers.
- Using triptans, NSAIDs, or combination painkillers too often can cause rebound headaches.
- General rule: limit acute medications to no more than 2 days per week unless your doctor advises otherwise.
5. Know Your Options
If one medication fails, another may still work. For example:
- If one triptan doesn’t help, another triptan may.
- If oral drugs fail due to nausea, ask about injectable or intranasal options.
6. Keep a Medication List Handy
Having your current and past medications in one place helps avoid mistakes, especially in emergency settings.
Many people find it useful to carry a wallet card or keep a printable checklist to show doctors.
>> Pro Tip: My Printable Migraine Medication List makes this easy. You can download and fill in your current medications, doses, and what has (or hasn’t) worked - so you’re always prepared.
Resources & References
These resources provide more in-depth, medically reviewed information on drugs for treatment of migraine and acute treatment strategies:
- American Migraine Foundation - patient-friendly guides on acute and preventive medications.
- Mayo Clinic: Migraine Treatments - overview of prescription and OTC options.
- National Institute of Neurological Disorders and Stroke (NINDS) - research-based information on migraine.
- NHS Migraine Treatments - UK-based resource on medication safety and options.
Always review treatment decisions with your prescribing physician or specialist.
Click here to download and print the PDF for the NSW Therapeutic Assessment Group (2002) Migraine publication for prescribing guidelines for primary care physicians.
Frequently Asked Questions (FAQ)
1. What’s the difference between acute and preventive migraine medications?
1. What’s the difference between acute and preventive migraine medications?
Answer: Acute medications are taken at the start of an attack to stop the progression of the migraine cycle and or reduce pain in the headache phase. Preventive medications are taken daily to reduce the frequency and severity of future attacks.
2. How do I know if I’m overusing my migraine medications?
2. How do I know if I’m overusing my migraine medications?
Answer: Using triptans, NSAIDs, or other pain relievers more than 10–15 days a month can cause medication overuse headache (MOH). Track usage and review with your doctor.
3. What drugs for treatment of migraine work best for fast relief?
3. What drugs for treatment of migraine work best for fast relief?
Answer: Often, a combination of fast-acting pain relievers (like ibuprofen) with longer-lasting triptans (such as naratriptan) provides stronger and more sustained relief. Always confirm safe combinations with your doctor.
Ready to take the next step?
Choose the next step that fits where you are right now.
MIGRAINE MEDICATIONS Related Articles
Drugs for Treatment of Migraine Reference: NSW Therapeutic Assessment Group (2002) Migraine.
[Online], No longer available at:
http://www.ciap.health.nsw.gov.au/nswtag/publications/guidelines/Migraine41202.pdf