GET THE BEST MAGNESIUM!
My #1. Magnesium Breakthrough by BiOptimizers – combines 7 types of magnesium in a humic/fulvic monoatomic blend to optimize absorption. This is by far the best product I have found so far in terms of results.
Menopause Headaches: What You Need To Know
 Menopause headaches: causes, triggers, symptoms, successful treatment and alternative solutions @migrainesavvy
Menopause headaches: causes, triggers, symptoms, successful treatment and alternative solutions @migrainesavvyHow do you stop menopause headaches?
A question I get asked a lot is "when will my menopause headaches stop? I thought I'd be migraine free after menopause, but they are carrying on and on."
Well, do you want the good news or the bad news first?
My #1 Choice in Magnesium Supplements
The bad news is... there's no guarantee that your migraines will stop with menopause.
I know, it's not the answer you're waiting for. You want a resounding "yes your migraines will definitely stop after menopause." There are no more fluctuating hormones, so there's a really good chance they will stop.
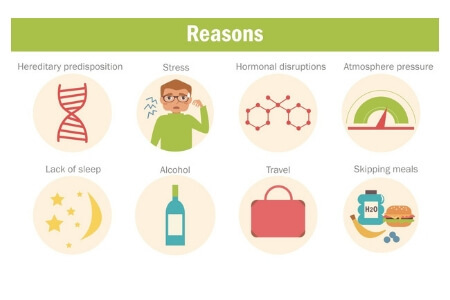
The problem is that hormones may not be your only cause or your only trigger. The most well known phase of a migraine is the painful headache. But the causes and triggers are different things all together.
Not everyone has exactly the same combination of triggers. You might be more reactive to: food intolerances, allergies, or glare. While I am triggered by: smells (smoke, perfume, incense) and hormones. Other triggers are menopause, stress, the weather... the list goes on.
Or an injury may be the cause of your headaches.
Migraines can be frightening and can impact your life in so many ways. The more severe and chronic the attacks, the more destruction they can cause in your life.
I prayed for menopause to come early for me in the hopes of stopping my migraines. It didn't come early but they did stop. And I count myself VERY lucky.
So my friend, you might be blessed and the migraines tone down to more gentle menopause headaches that are easy to manage, or they might completely disappear.
Or the headaches can start in or after menopause, when you've never had them previously.
Keep reading... here are some things you need to know.
What causes the headaches?
Some research says that approximately 50% of women struggle with migraines during their menstrual cycle. And other reports say 90%. Either way you look at it, it's a lot.
The menstrual cycle is associated with biological changes that are occurring in the body.
These chemical changes have a widespread effect on the body.
Some of us are more sensitive to changing hormone levels during the monthly cycle then others.
By now you may already know if the migraine attacks are linked to your periods.
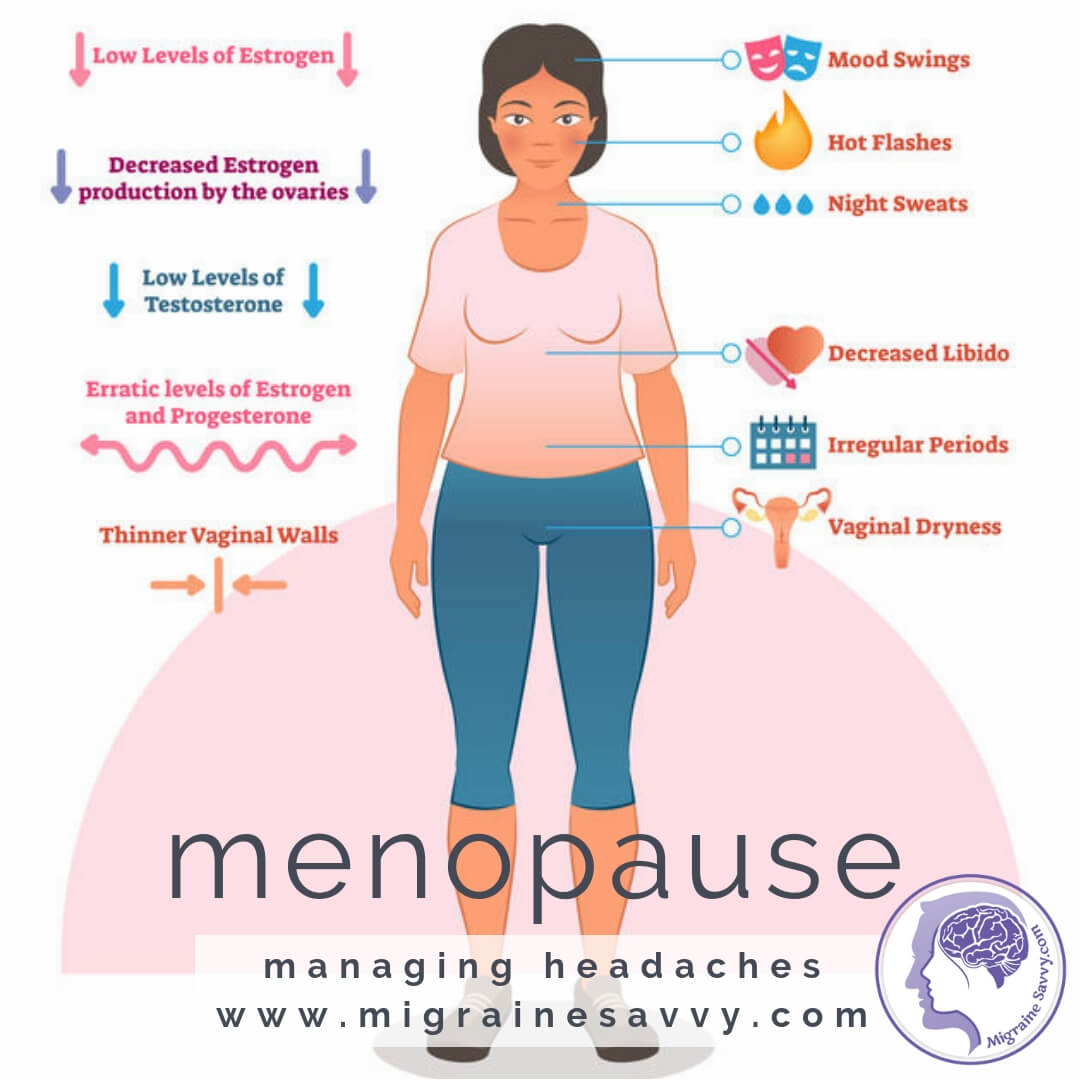
With the onset of menopause, we become less fertile, our estrogen production slows down. And the ovaries slowly stop producing eggs each month until the cycle stops completely.
The transition period in between our period becoming irregular and then stopping is called Perimenopause.
This process can last ten years. I know, I’m sorry to be the one to tell you this. Some women breeze through this transition. Some of us suffer.
Perimenopause can last 10 years. Migraines can become more frequent.
The average age to start menopause is 51 or 52 years of age. But some women start experiencing symptoms as early as 40 years old and others may not reach it until 60.
My perimenopause started at the age of 32, so it was more than ten years for me. Your migraine attacks during this period of time can become more frequent and severe due to the fluctuating hormone level production. Or they just might become less frequent, or less severe.
Did you know that your hormonal changes can act as your migraine triggers for as long as two to five years after menopause? So that's... before menopause... during menopause... and after menopause.
All of your other non-hormonal type triggers might seem more obvious now. And the changes in your periods can make it harder to cope with your migraines as they can be harder to predict than when you had a regular cycle.
This is the last bit of bad news, you know the hot flushes and night sweats that are associated with menopause? They can be triggers to set off more migraine attacks as well. You might experience menopause headaches from disturbed sleep and more bodily stress at this time in your life.
So they are less predictable; you can become more sensitive to things as you age; your symptoms can also be triggers.
triggers...
- hormonal fluctuations
- decreased estrogen production
- injury
- eye strain, glare
- increased sensitivities: food, allergy, smells
- stress
- disturbed sleep
symptoms...
- mood swings
- hot flushes
- night sweats
- loss of libido
- memory loss
- headaches
- migraines
triggers...
- hormonal fluctuations
- decreased estrogen production
- injury
- eye strain, glare
- increased sensitivities: food, allergy, smells
- stress
- disturbed sleep
symptoms...
- mood swings
- hot flushes
- night sweats
- loss of libido
- memory loss
- headaches
- migraines
"Menopause can last as long as twenty years." [3]
Don't despair, there is good news.
Want expert help with your migraine attacks... for FREE?
What You Need To Know For Successful Menopause Headache Treatment
Hormone Replacement Therapy (HRT) is often used to successfully treat the symptoms of menopause. There is not a lot of research linking HRT with migraine headaches. It might be trial and error to see what your body needs for balance.
You can also consider natural or traditional hormone treatments. Either way, trying to balance your hormones may come with risks.
Consult with your physician, if you feel the need for hormone replacement. Health history and family health history need to be taken into consideration before starting hormone therapy.
A rather large study with over 22,000 doctors, who also had migraines found the risks leaned more towards stroke than heart attacks.
I covered this thoroughly in reducing migraine stroke risks. The study followed the doctors over years, so the findings feel reliable to me.
Once you and your doc both decide it is the right path to take, it is very important to take the hormones long enough to give your body the time it needs to adjust to the meds. Unless you have side effects, of course.
Try different delivery methods for taking the hormones in order to find the best course of treatment for you. Here are some options:
- capsules, sublingual lozenges, patches, gel, topical creams and suppositories.
Note: oral capsules or tablets have to pass through your digestion process so their effectiveness may be compromised. Creams, suppositories and sublingual troches are forms of transdermal absorption, all of which bypass the digestive system.
I've written more about what bioidentical hormones to consider experimenting with here - Are Balanced Hormones A Cure For Migraine Headache?
Drug Free Alternatives To Help Stop Menopause Headaches
The good news is that there are herbal non-drug treatments available that help with other symptoms like:
- Black Cohosh
- Chasteberry (Agnus Castus)
- Ginkgo Biloba
- Evening Primrose Oil (EPO)*
- Dong Quai
- Red Clover
- Ginseng
- Kava
And vitamins like:
- St. John's Wort
- Selenium and
- Vitamin C
Note: be careful with EPO as it can also increase menopause headaches and migraines.
And if you suffer with weight gain, you might like to try taking some MCT oil everyday. It's great for energy too. I use this one - Bulletproof Brain Octane Oil.
And changing your lifestyle to incorporate meditation and exercise is always beneficial to help stop menopause headaches.
If you are able to see a specialist, they should be able to tell you (or remember to ask them) their best results with treating menopause headaches and symptoms like yours.
Keep trying until you find what works.
Want expert help with your migraine attacks... for FREE?
Will A Hysterectomy Stop The Relentless Pain?
This is another question I get asked a lot.
If removing your ovaries through a hysterectomy is required because of medical reasons, the resulting menopause does not typically improve migraines and studies show it will more than likely make them worse.
Dr. Susan Hutchinson, Director of Orange County Migraine & Headache Center, in Irvine, CA. in her article for AMF says that surgical menopause from having a hysterectomy causes an immediate dramatic drop in hormones. In two out of three women, it will make their migraines worse.
Her statistics showed that two out of three women (66.67 percent) will experience improvement in their migraine if they go into menopause naturally.
So whether you enter menopause forcibly from surgery or go into it naturally will make a difference. It will determine how much you are affected in the process.
The end of the natural menopause can often be a good time for a woman who suffers from migraines. Menopause can often mean a reduction in migraine frequency, severity and duration.
Try to keep medications to a minimum. With the aging process your body doesn't tolerate drugs as well, especially if you are taking medications for other medical issues.
If, later in life, you start to suffer from migraines or experience a change in the pattern of your present migraines, be sure to let your physician know asap.
Here Are Some Key Points For Clarity
- The average age for menopause is 51 to 60. But it can start at 40.
- Having a hysterectomy will not stop migraine attacks. In fact it could make them worse.
- If you go through menopause naturally you have a better chance at them stopping.
- If you've never had migraines, you could start getting headaches during or after menopause. Even 5 years after.
- Hot flushes, stress and poor sleep can trigger more headaches.
- Meditation and exercise are very beneficial.
- You might be in this for a long time, so make sure to be kind and gentle to yourself. I have some great stress reduction tips in my book - Migraine Management... take a look.
If you like this article... please share it.
Come back and visit soon,
WANT MORE TIPS? Subscribe to my newsletter and follow along on Facebook and Pinterest for all of the latest updates.
MIGRAINE CAUSES Related Articles
How to be more migraine savvy right now...
Menopause Headaches References:
1. Hutchinson, Susan MD (AMF) Hysterectomy and Migraine: What can you expect? [Online] Available. Updated Oct. 23, 2018.
2. WebMD (2018) Migraines and Menopause. Available [online] at: https://www.webmd.com/migraines-headaches/migraines-menopause#2
3. The Migraine Trust (2018) Menopause and midlife. Available [online] at: https://www.migrainetrust.org/about-migraine/trigger-factors/menopause-and-midlife/