- Home
- Your Stories
- What Causes Pain at the Back of the Head
What Causes Pain at the Back of the Head?
 Can pain at back of head be a migraine? Yes, it can @migrainesavvy
Can pain at back of head be a migraine? Yes, it can @migrainesavvy
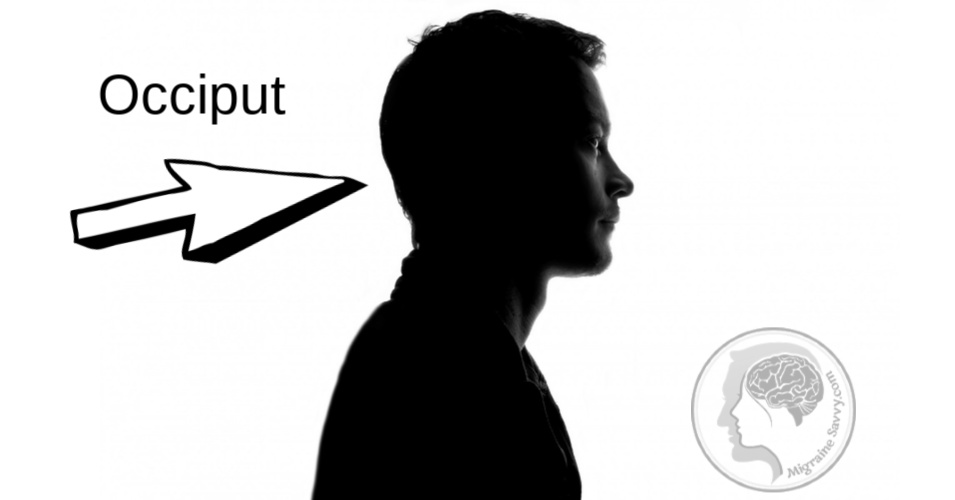
Few things are more alarming than unexplained head pain. Pain at the back of the head in migraines is common. The nerves are over excited before and during an attack so this might be the first place you feel an attack is on its way.
Pain at the back of your head can also be from other things like: arthritis, poor posture, herniated disks (cause Cervicogenic headaches that may intensify when you lie down), or occipital neuralgia, to name a few. [1]
Occipital neuralgia is caused when the occipital nerves, that run from the top of the spinal cord up through the scalp, are injured or inflamed. If this happens you can feel pain in the back of your head or the base of your skull. [2]
Because the symptoms are so similar to migraines and other types of headaches, it's easy to get confused. Make sure to see your doctor. If you get pain that feels like a "sharp, jabbing, electric shock" in the back of the head and neck, it might indicate occipital neuralgia. [2]
Also watch for: burning, throbbing or aching that starts at the base of the head and goes to your scalp on one or both sides of the head. [2]
Here's one woman's personal account of occipital neuralgia in the comments section below.
If you get pain that feels like a dull, tightness... that might indicate a tension headache.
If you get pain at the back of the head that is one sided, severe and throbbing and accompanied by these:
- blurry vision (aura)
- nausea or vomiting
- watering eyes
- sensitivity to light, sound or smell
This would indicate a migraine headache. Either way, pain at the back of the head should take you straight to your doctor to get a diagnosis. And if that stresses you out, here's what Carol, one of my readers, does to help reduce the stress.
My #1 Choice in Magnesium Supplementation
3 Ways To Combat Head Pain From Stress
~ A guest post by Carol (USA)
Hello everyone,
My name is Carol and I am fairly new to this migraine stuff.
I am a school-teacher and I’ve had migraines for almost 3 years.
It all started with just a short sharp pain at the back of my head, on the right side. Then it just got worse until I could not see clearly. Nothing I took seemed to reduce the pain. And then the vomiting came. Oh, so much vomiting.
I was diagnosed in an off-hand manner (almost dismissed) by my doctor nearly 2 years ago, but it took me until 4 months ago before I understood and began accepting the diagnosis. Between attacks I am fine, happy with life, but I struggle during, as I imagine most of us do.
I think I might still be in denial of this long term condition. I live in hope they will just go away.
I have come to the conclusion that stress is my major trigger of symptoms and crashes into an attack.
I wanted to share what I do to reduce stress now:
1. Train Yourself To Relax... Every Day
Each and every day, I practice relaxation/meditation/self-hypnosis, often with the guidance of recordings. I do this twice a day, late morning and late afternoon or early evening, for roughly 20 to 25 minutes each time.
I find this rejuvenating, and I think it not only reduces stress and gives me peace in the moment, but also is training me to be able to relax and also sleep more consciously and quickly when I need to as inevitable expected and unexpected stresses arise.
2. Pay Attention To When You Feel Joy
This may sound a bit clichéd, but during the hours or days when I’m feeling good, I notice myself feeling a sense of joy that I didn’t have when I could take feeling good for granted! When I notice this, I pay attention to it and really appreciate life.
3. Tune Into Nature
I look for and pay attention to the small and larger beauty of nature. This could mean taking in the view around me at home, where I’m lucky to live in quite a beautiful place; it could mean (as now) noticing the crocuses and daffodils just beginning to bloom; it could mean enjoying watching my adolescent dog provoke my adult dog into playing and racing around in circles.
Looking at nature just for a few seconds can relax you and bring a sense of peace.
More than these three: I also am never without a novel; I exercise, which definitely reduces stress; and I write, which allows me to lose myself in my characters and their lives... great fun.
I hope this helps other sufferers cope with their migraines and stop triggers of stress. I have learned I need to make this the most important part of my day.
Bringing joy to myself brings peace and more energy to cope with the ruthlessness of the migraine attacks.
With much love,
Carol
Deal with stress by: exercising, write in a journal or write a novel, and find what feels like great fun.
Stay in touch...
BE INFORMED. STAY INFORMED. JOIN THE MAILING LIST.
Ready to take the next step?
Choose the next step that fits where you are right now.
MIGRAINE STORIES Related Articles
Comments On Pain at Back of Head
My Health History, Pain at Back of Head Diagnosed as Occipital Neuralgia and Migraines by Jennifer (NJ, USA)
Well I have had migraines since high school, on and off. I am currently a 29 yr old female from NJ. Over the past 3 months the attacks have become debilitating. I am no longer working as a dental assistant, which I loved. I am married; we've been together for about 4 yrs; no kids. He has already seen me through ovarian cancer in 2009, I am well and over that! : ) I also suffer from mild epilepsy and mild depression since high school.
Over the past 3 months I've had non-stop searing pain. I was diagnosed with occipital neuralgia on the right side. Why or how... who knows? I've tried the following to no avail: heat, ice, lots of sleep, little sleep, lavender oil, quercetin, co enzyme, B12 , skull cap, feverfew, butterbur, magnesium, multivitamin, Flerexil, Zanaflex, Fioricet, 3 occipital injections, 1 supra injection, a 6 day steroid pack to calm the nerve.
But wait... there's more: Imitrex, lotion no. 10 numbing cream, drinking lots of water until I had clear pee, acupuncture, chiropractic, changing my diet - no caffeine at all. I never really drank soda or coffee. No chocolate. I tried upping my protein, even though my blood tests said my vitamin levels & blood counts were normal, blood pressure is very good. I am happy about that.
So what in the world is causing it? Yes my body mass index is over, I am a bit on the heavy side, certainly not obese. I've also lost weight to try and help but that didn't either.
So where has taking all these different pain pills left me? I don't take them unless I have to. I know how they work, all of them just lead to having to take more and higher doses. My biggest fear is becoming like my father who was addicted to pain pills for his back. The small amounts I have taken to dull the pain have left me tired and unable to do basic tasks.
My mind, these past few months, has made me become a monster. I'm flying off the handle at the smallest of things my usual self would just brush off. I have hit a wall, a window, and threw down a fan. These things are not me. It's the constant pain causing anger in me to lash out at I can't even remember what. I am also suffering short term memory loss. But the scariest is this sudden blind rage. I am not mad all the time I just feel extremely guilty for these 'moments' I do have. My husband is truly wonderful and my best friend.
So my next step is my pain management. My Doctor wants to 'burn the optic nerve' further down, I believe it's called a rhizotomy. This does cause a numbing of one side of ones' scalp. The procedure is a series of 3 injections done under twilight anesthesia. Sometimes this nerve grows back... sometimes it grows back fine, sometimes with pain. Out of 200 patients my Doctor has had only one in which it ever grew back, and in this particular patient it did cause pain again. So you would just get it 're burned'.
I have looked everywhere online for videos on this procedure, it's very frustrating the lack of understanding & overall information available to people. Well I have a numbing test next week to see if I qualify for this rhizotomy in the first place, if I don't well.... well now what else? (I hope this all made sense I wrote it with a migraine!)
Depression From Occipital Neuralgia Treatment Not Working by Jennifer
Since the occipital neuralgia treatment - the right side nerve burning surgery - I have had electric shocks all along the right side of my head. My pain management Doctor assured me that this was normal and would subside. It's now three months later and the pain is less frequent, but sometimes I feel it all day long which is annoying.
My migraines have returned but with less frequency - sadly the same level of pain. So I was put on Lyrica (75 mg). In conjunction with that the Doctor wants to try one more supra orbital injection even when the other 3 didn't work.
I have resigned myself to do what he says. If the injection and Lyrica do not work then next step is an implant in my head/chest that stimulates stuff in my brain when pain comes along. Shock and horror spread across my face when the doctor suggested this treatment. I am feeling apathetic, depressed, and hopeless about this whole thing - if you cannot tell that already. So since my last treatment 3 months ago, depression has hit me hard.
I went to my psychiatrist who has changed my medications a few times. It's amazing how a simple change in dose, just a few milligrams can make my negative harmful thoughts just vanish!!
Another Occipital Neuralgia Treatment... Will This One Work? by Jennifer
Well it's scheduled - my second twilight surgery will be on May 24th. I have been told that recovery time is just coming out of anesthesia, like the other injections I've already had. I've had other surgeries but this one makes me nervous. I have to be awake to tell the Doctor if he's stimulating the right nerves 'in the right spot'... this sounds terrifying.
In the procedure, he will burn up the 3 areas, and then the results should be no more occipital migraines and cluster headaches. Have I mentioned both? Anyway, it's going to be a nice bonus combo to have an end to the pain.
Pain at Back of Head Resources:
1. Healthline (2018) Pain at Back of Head. Available [online] at: https://www.healthline.com/health/pain-in-back-of-head. Accessed December 2018.
2. WedMD (2018) Occipital Neuralgia. Available [online] at: https://www.webmd.com/migraines-headaches/occipital-neuralgia-symptoms-causes-treatments#1 Accessed December 2018, updated Nov. 23, 2020.